Learn Your Way
to A Healthier Life

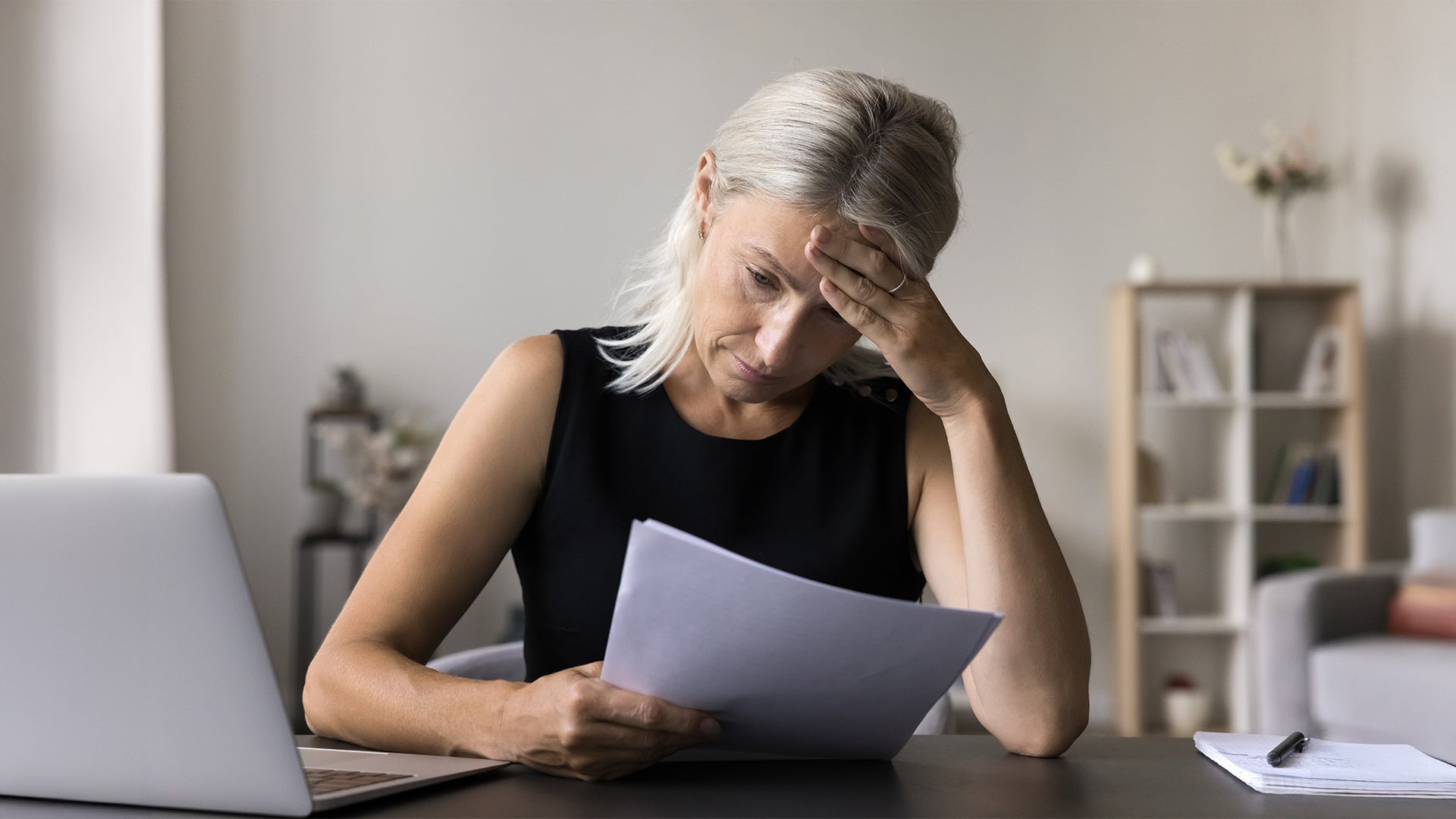
Stress, anxiety and depression can lead to unhealthy lifestyle choices, such as smoking, physical inactivity, poor sleep, excessive alcohol consumption and medication non-compliance. Over time, these behaviors can increase the risk of heart disease, hypertension and other cardiovascular issues.
The Science Behind Stress and Your Heart
The human body's stress response has evolved to protect it from danger. When someone encounters a stressful situation, their body releases stress hormones like cortisol and adrenaline. These hormones trigger "fight or flight" responses, causing faster heart rate and rising blood pressure. While this response is helpful in truly dangerous situations, chronic stress can keep the human body in this heightened state for extended periods.
Over time, persistent stress can lead to:
- Elevated blood pressure
- Irregular heart rhythms
- Increased inflammation throughout the body
- Higher risk of blood clots
- Weakened immune system
When Anxiety Weighs on Your Heart
Anxiety disorders are the most common mental illness in the US, affecting 40 million adults over the age of 18. Their impact extends far beyond emotional distress. When someone experiences anxiety, their body goes through physical changes that can have the following effects on their cardiovascular system:
- Rapid heart rate (tachycardia). In serious cases, this interferes with normal heart function and increases the risk of sudden cardiac arrest.
- Increased blood pressure. If chronic, this can lead to coronary disease, weakening of the heart muscle and heart failure.
- Decreased heart rate variability. This may result in higher incidence of death after an acute heart attack.
A study published in Current Psychiatry Reports found that individuals with anxiety disorders had a 26% higher risk of developing coronary artery disease (CAD). The constant state of alertness and worry can lead to unhealthy coping mechanisms, such as smoking, overeating or alcohol use, which further increase cardiovascular risks.
Depression and Cardiovascular Risk
Depression is a significant risk factor for heart disease, with an American Heart Association (AHA) study showing that individuals with depression are twice as likely to develop cardiovascular issues. Depression affects various biological processes that impact heart health:
- Increased inflammation throughout the body
- Changes in blood clotting
- Disrupted sleep patterns
- Altered hormone levels
- Reduced heart rate variability
Depression can also lead to behaviors that increase cardiovascular risk:
- Reduced physical activity
- Poor dietary choices
- Medication non-compliance
- Social isolation
- Increased substance use
Managing Stress, Anxiety and Depression for a Healthier Heart
Mitigating mental health challenges can improve cardiovascular outcomes. Here are some strategies to promote both mental and heart health:
Mindfulness and Meditation
Deep breathing exercises, progressive muscle relaxation and guided imagery can help calm the nervous system and reduce stress in addition to lowering blood pressure, reducing cortisol levels and improving overall heart health.
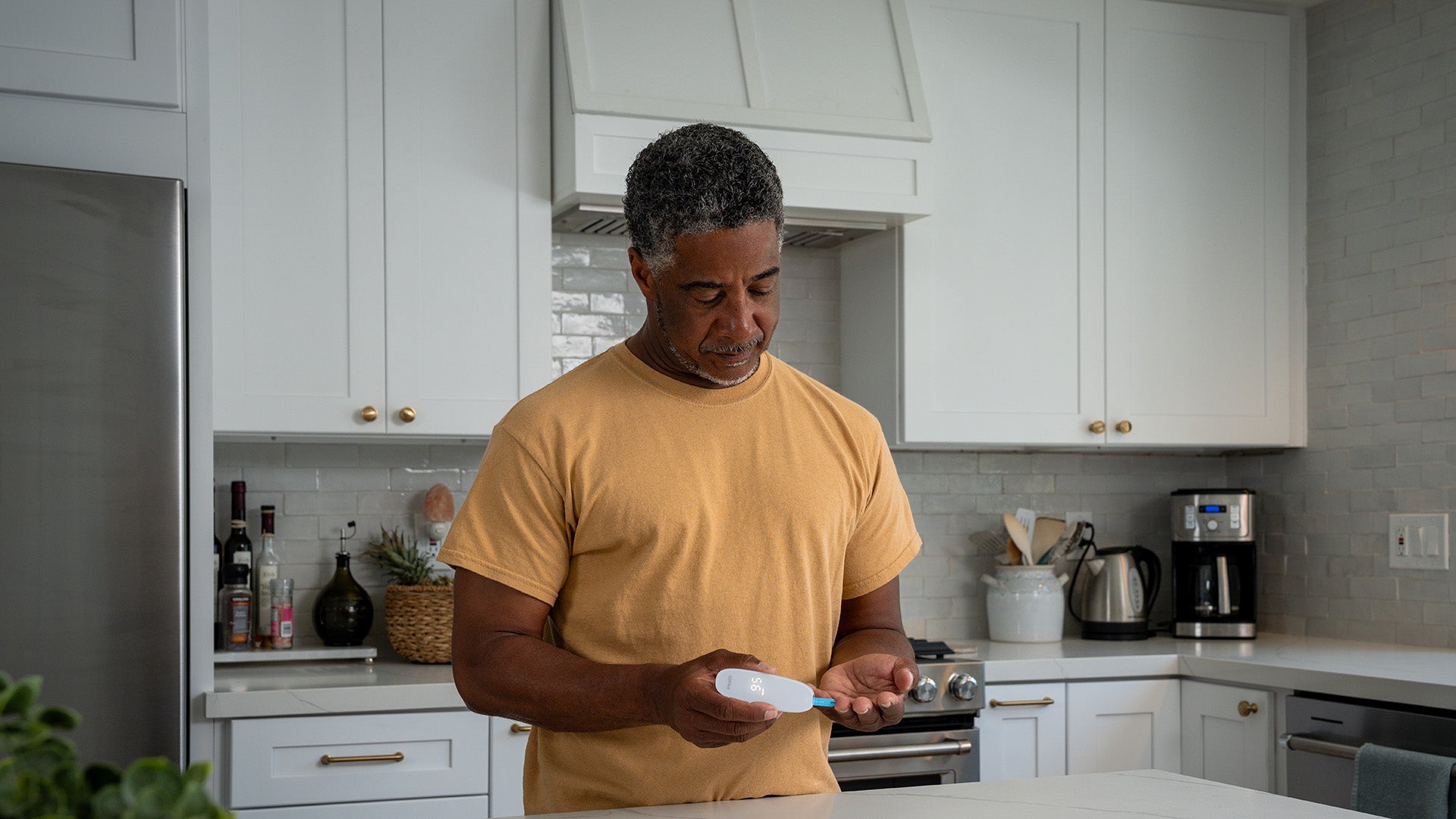
Regular Physical Activity
Exercises like walking, swimming, yoga and cycling are some of the most effective ways to manage stress, anxiety and depression while benefiting the heart. The AHA recommends at least 150 minutes of moderate-intensity exercise per week for cardiovascular health.
Healthy Diet
A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins and healthy fats supports both mental and physical well-being. The Mediterranean diet, which focuses on plants and traditional flavors and cooking methods of the people in the Mediterranean region, has been linked to lower rates of depression and reduced cardiovascular risk.
Social Support and Therapy
Connecting with friends, family and support groups can alleviate stress and foster emotional resilience. Therapy, including cognitive-behavioral therapy (CBT), has been shown to be effective in managing anxiety and depression, indirectly benefiting heart health.
Adequate Sleep
Poor sleep is associated with both mental health disorders and cardiovascular disease. Seven to nine hours of quality sleep each night allows the human body to recover and regulate stress hormones effectively.
While traditional risk factors like high cholesterol and smoking are well-known, mental health is just as critical in maintaining a healthy heart. By recognizing the impact of mental health on heart health and implementing lifestyle changes, individuals can reduce their risk of heart disease and improve overall well-being. Seeking professional help, prioritizing self-care and adopting heart-healthy habits can pave the way for a healthier and more fulfilling life.
References
- Mayo Clinic - Chronic stress puts your health at risk
- Yale Medicine - Yes, Stress Can Hurt Your Heart: 3 Things to Know
- Anxiety & Depression Association of America - Anxiety Disorders - Facts & Statistics
- Johns Hopkins Medicine - Anxiety and Heart Disease
- Current Psychiatry Reports - Anxiety disorders and cardiovascular disease
- AHA - Depression and Coronary Heart Disease
- Johns Hopkins Medicine - Depression and Heart Disease
- Journal of the American College of Cardiology - Screening and Management of Depression in Patients with Cardiovascular Disease
- AHA - What Exercise Is Right for Me?
- Psychiatry Online - Cognitive-Behavioral Treatments for Anxiety and Stress-Related Disorders
Sign Up For More From iHealth
Receive the Latest News and Special Offers