Learn Your Way
to A Healthier Life

March is National Kidney Month, a time when healthcare providers, patients and advocacy groups unite to raise awareness about kidney health and chronic kidney disease (CKD). Our kidneys play a vital role in filtering waste and excess fluids from the blood in our bodies—regulating blood pressure, balancing electrolytes and producing hormones essential for red blood cell production and bone health.
Chronic kidney disease (CKD) is a progressive condition characterized by the gradual loss of kidney function over time. This often-silent condition affects millions of Americans, with many unaware they have it until significant damage has occurred. When kidney function declines, it can lead to a buildup of waste products in the body, leading to health complications that can affect nearly every system in the body.
However, targeted management strategies—in particular, controlling blood pressure, managing blood glucose levels and maintaining a healthy weight—can slow the progression and improve outcomes for those living with CKD.
Understanding CKD

CKD is categorized into five stages, ranging from mild kidney damage in stage 1 to complete kidney failure in stage 5. The progression of CKD through these stages is often gradual and may go unnoticed until significant kidney function has been lost. Early detection and management are vital to prevent or delay the onset of end-stage renal disease (ESRD), where dialysis or kidney transplantation becomes necessary. This makes preventive care through regular screenings especially important for those at higher risk, including people with:
- Hypertension (high blood pressure)
- Heart disease
- Diabetes
- Obesity
- Family history of kidney disease
How Blood Pressure Affects Your Kidneys
High blood pressure (hypertension) is both a cause and a consequence of CKD. Elevated blood pressure can damage the blood vessels in the kidneys, reducing their ability to function properly. Conversely, impaired kidney function can lead to increased blood pressure, creating a detrimental cycle that accelerates kidney damage.
For people with CKD, blood pressure targets are typically lower than for the general population. The American Heart Association and National Kidney Foundation recommend maintaining blood pressure below 130/80 mmHg (millimeters of mercury—measurement of blood pressure) for most patients with kidney disease.
Strategies for controlling blood pressure include:
- Taking prescribed medications consistently
- Lowering sodium intake to less than 2,300 mg daily
- Regular physical activity (aim for 150 minutes of moderate activity weekly)
- Limiting alcohol consumption
- Quitting smoking
- Practicing stress reduction techniques
Even modest blood pressure decreases can significantly slow CKD progression. Studies have shown that each 10 mmHg reduction in systolic blood pressure can lower the risk of kidney disease progression by 22%.
Blood Glucose Management for CKD and Diabetic Kidney Disease
Diabetes is the leading cause of CKD. High blood glucose levels can damage the kidneys over time, leading to diabetic kidney disease or diabetic nephropathy—a specific type of kidney disease resulting from diabetes. Managing blood glucose levels effectively is crucial in slowing the progression of CKD for individuals with diabetes.
High blood glucose levels force kidneys to filter more blood than normal, putting extra strain on the kidneys’ filtering units (nephrons). Over time, this burden damages these structures, allowing protein to leak into the urine—often the first sign of diabetic kidney disease.
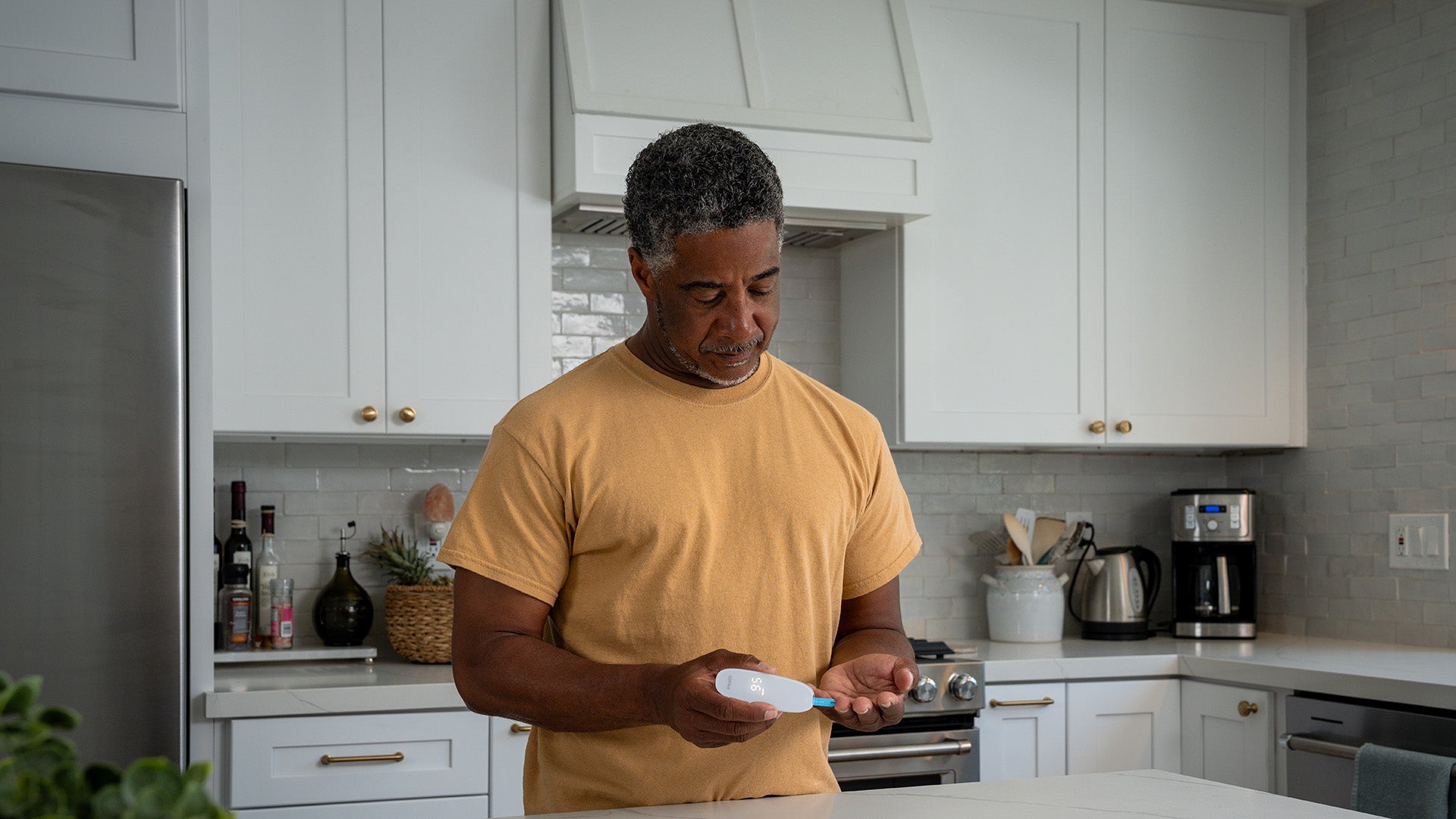
Those with diabetes and CKD can control their glucose by:
- Monitoring blood glucose regularly
- Taking diabetes medications as prescribed
- Working with healthcare providers to maintain target A1C levels (typically below 7% for most patients, though individualized targets may vary)
- Following a balanced diet developed with a dietitian
- Staying physically active
- Attending regular check-ups to monitor both diabetes and kidney health
Emerging therapies such as Sodium-Glucose Cotransporter 2 (SGLT2) inhibitors have shown promise in improving kidney outcomes. These medications work by blocking glucose reabsorption in the kidneys, leading to glucose excretion in the urine. Clinical trials have demonstrated that SGLT2 inhibitors reduce the risk of kidney failure and slow the progression of kidney disease in individuals with type 2 diabetes.
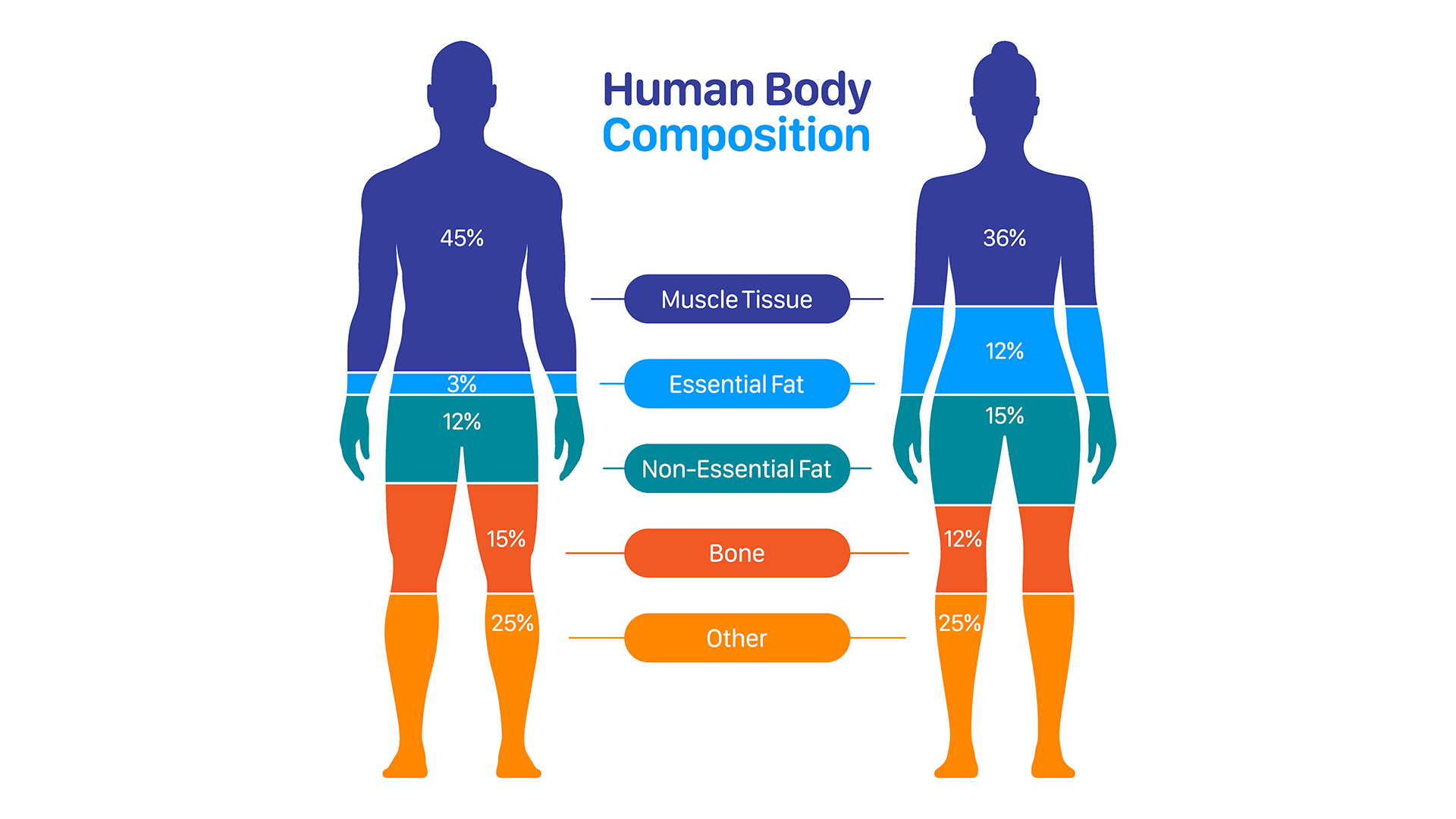
Weight Management for Mitigating CKD
Obesity is a significant risk factor for developing CKD and can exacerbate existing kidney disease by:
- Increasing blood pressure
- Worsening insulin resistance and diabetes control
- Causing inflammation throughout the body
- Placing mechanical stress on the kidneys
- Altering hormonal balance
A study published in the Journal of Renal Nutrition found that combining dietary changes, physical activity and weight management slowed kidney function decline by nearly 40% in patients with moderate CKD. Incorporating whole grains, fruits, vegetables and lean proteins while limiting processed foods and added sugars can support a healthier weight and improved kidney function.
The most effective CKD management combines blood pressure control, glucose monitoring and weight maintenance—along with medication adherence. By adopting these strategies and working closely with healthcare providers, patients can slow CKD progression, reducing the risk of complications and improving long-term outcomes.
References
- Mayo Clinic - Chronic Kidney Disease
- National Institute of Diabetes and Digestive and Kidney Diseases - Slow Progression & Reduce Complications
- American Kidney Fund - Stages of Kidney Disease
- National Institute of Diabetes and Digestive and Kidney Diseases - High Blood Pressure & Kidney Disease
- Canadian Medical Association Journal - Effects of intensive blood pressure lowering on the progression of chronic kidney disease
- National Institute of Diabetes and Digestive and Kidney Diseases - Diabetic Kidney Disease
- Renal Replacement Therapy - SGLT2 inhibitors in peritoneal dialysis
- Canadian Journal of Kidney Health and Disease - Obesity and Kidney Disease
-
Journal of Renal Nutrition - Association Between Dietary Patterns and Kidney Function in Patients With Chronic Kidney Disease
Sign Up For More From iHealth
Receive the Latest News and Special Offers