Learn Your Way
to A Healthier Life

World Health Day, observed annually on April 7th, serves as a global platform to raise awareness about pressing health issues affecting communities worldwide. The World Health Organization (WHO) has announced that the theme for World Health Day 2025: "Healthy Beginnings, Hopeful Futures" will serve to raise awareness of the significance of maternal and newborn health. This focus emphasizes the need to ensure that every mother and child has access to quality healthcare, paving the way for flourishing societies.
One significant health concern impacting maternal and newborn outcomes is diabetes during pregnancy. Diabetes, particularly when not properly managed, poses serious risks to both mothers and their infants, contributing to increased mortality and long-term health complications.
Diabetes during pregnancy can manifest in two forms: pregestational diabetes and gestational diabetes mellitus (GDM).
Pregestational diabetes refers to women who have either type 1 or type 2 diabetes prior to their pregnancy. Pregestational diabetes affects approximately 16% of pregnancies globally.
Gestational Diabetes Mellitus (GDM) is characterized by elevated blood sugar levels that develop during pregnancy in women who did not previously have diabetes. GDM typically arises in the second or third trimester and affects how cells use glucose, leading to hyperglycemia, impacting up to 15% of pregnancies globally. While GDM can often resolve after childbirth, it poses immediate and long-term risks for both mother and child.
Growing Diabetes Concerns in Maternal Health
Uncontrolled blood glucose levels during pregnancy can lead to numerous issues, including:
- Preeclampsia, a pregnancy complication characterized by high blood pressure
- Higher rates of cesarean deliveries
- Increased risk of maternal mortality
- Greater likelihood of preterm birth, when babies are born alive before 37 weeks of pregnancy are completed
These aforementioned problems contribute significantly to maternal mortality rates, with diabetic mothers being three times more likely to experience severe difficulties during pregnancy compared to non-diabetic mothers. Increases in GDM were seen in each maternal age group, and rates rose steadily with maternal age—during 2021, the rate for mothers 40 years and older (15.6%) was nearly six times as high as the rate for mothers under 20 years old (2.7%).
How Diabetes Impacts Newborns
The effects of maternal diabetes extend well beyond the mother's health, significantly impacting newborns as well. Babies born to mothers with poorly controlled diabetes face immediate health challenges, including:
- Congenital malformations
- Macrosomia, or excessive fetal growth
- Hypoglycemia, or low blood sugar levels
- Respiratory distress syndrome
- Increased risk of stillbirth and neonatal death
The Journal of Developmental Origins of Health and Disease has reported that children born to mothers with diabetes have higher lifetime risks of developing obesity, type 2 diabetes and cardiovascular disease themselves—creating a concerning cycle of intergenerational health challenges.
Disparities in Diabetes Care
One of the most troubling aspects of the diabetes-maternal health crisis is its uneven distribution across populations. Low and middle-income countries bear a disproportionate burden, with maternal mortality rates from diabetes-related complications up to six times higher than in high-income nations. Even within wealthy countries, significant disparities exist along socioeconomic, racial and geographic lines.
Integrating Diabetes Management into Maternal Health Programs
Addressing diabetes effectively requires its integration into existing maternal and newborn health initiatives. Key strategies include:
- Policy developments with governments and health organizations which should establish policies that prioritize diabetes screening and management within maternal health programs.
- Training healthcare providers by enhancing their skills in diagnosing and managing diabetes
- Educating communities about diabetes for increased awareness and encouraging women to seek timely prenatal care
Promising Interventions and Approaches for Diabetes During Pregnancy
Despite the aforementioned challenges, significant progress has been made in understanding how to better care for pregnant women with diabetes. The International Journal of Integrated Care published a study on comprehensive care models that integrate diabetes management with prenatal care and how they have shown remarkable success in reducing complications. These include:
Early Screening and Intervention
Universal screening for gestational diabetes between 24-28 weeks of pregnancy has become standard in many healthcare systems, but early screening for high-risk women can identify issues sooner. Some healthcare systems have begun implementing first-trimester screening for women with risk factors, allowing for earlier intervention.
Multidisciplinary Care Team
While diabetes is typically a self-managed disease, a team-based approach involving obstetricians, nutritionists and endocrinologists can ensure most aspects of a woman's health are addressed throughout pregnancy. Endocrinologists, doctors who specialize in diagnosing and managing diabetes and other endocrine disorders, are especially important in helping patients understand and manage their conditions, prevent complications and improve their quality of life.
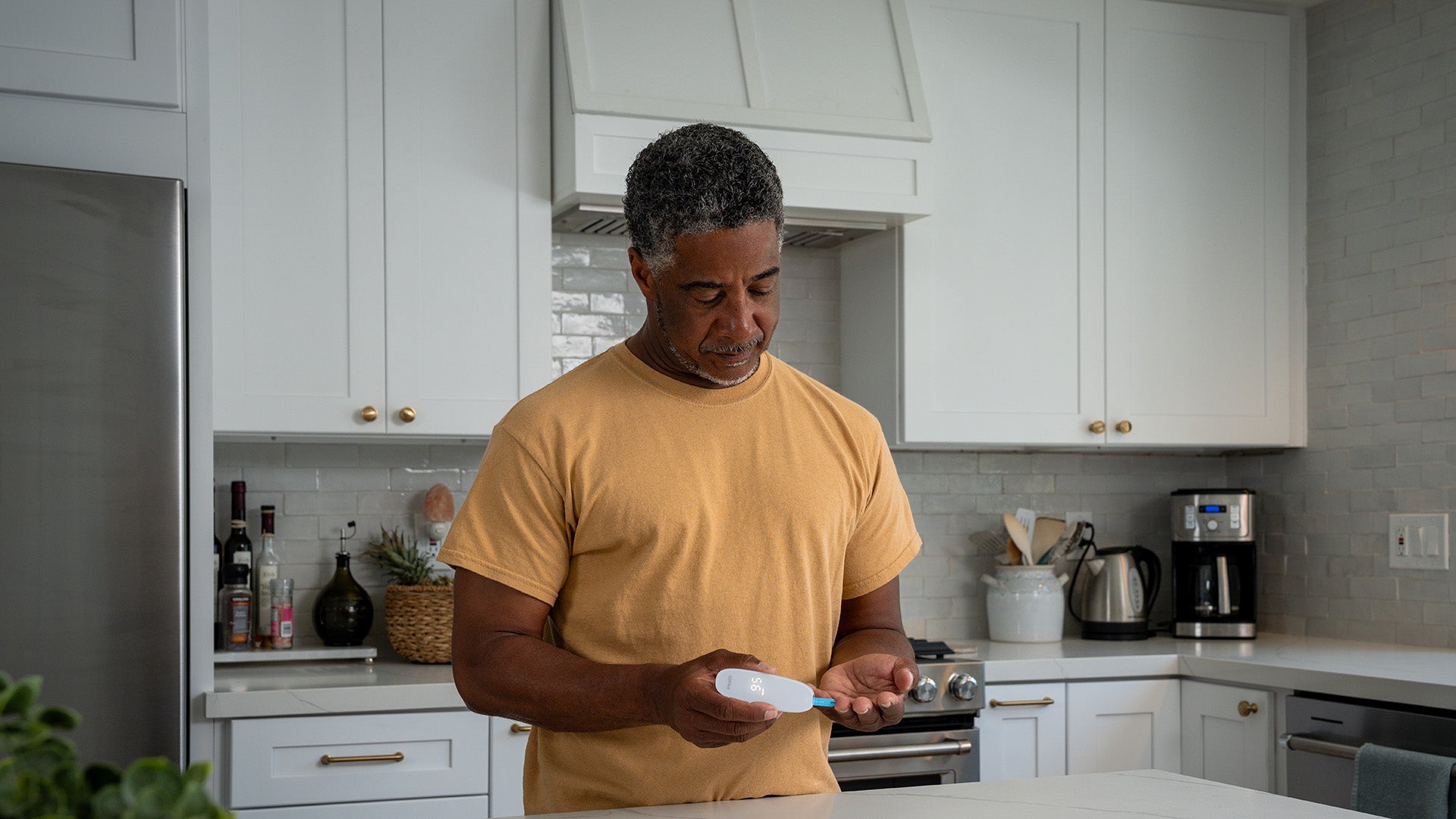
Glucose Monitoring Technology
Continuous glucose monitoring (CGM) systems have transformed diabetes management during pregnancy, providing real-time feedback and allowing for more precise insulin adjustments. Telemedicine has also expanded access to specialized care for women in remote areas, partially addressing geographic disparities.
Preconception Counseling
Women with pre-existing diabetes who receive comprehensive preconception counseling and achieve good glycemic control before becoming pregnant experience significantly better outcomes.
World Health Day 2025 serves as a powerful reminder that every mother and newborn deserves a healthy start in life. While diabetes during pregnancy presents serious challenges, early screenings, glucose monitoring and preconception counseling can help mitigate the risks associated with diabetes, improve clinical outcomes and break the cycle of intergenerational health challenges to ensure a future where every mother and child receives the care they deserve.
References
- BMC Pregnancy and Childbirth - Evaluation of neonatal and maternal morbidity in mothers with gestational diabetes
- Diabetes Research and Clinical Practice - The prevalence of pre-existing diabetes in pregnancy
- Journal of Clinical Medicine - Gestational Diabetes Mellitus
- CDC - Diabetes During Pregnancy
- Diabetology & Metabolic Syndrome - Adverse pregnancy outcomes in women with diabetes
- CDC - Birth Data
- Paediatrics and Child Health - Infant outcomes following diabetic pregnancies
- Cambridge Care - The impact of gestational diabetes and maternal obesity on the mother and her offspring
- International Journal of Integrated Care - Effectiveness of Integrated Diabetes Care Interventions Involving Diabetes Specialists Working in Primary and Community Care Settings
Sign Up For More From iHealth
Receive the Latest News and Special Offers