Learn Your Way
to A Healthier Life
 If you feel as if more people you know have come down with COVID-19 lately, it’s not just you. COVID-19 is on the upswing in many states.
If you feel as if more people you know have come down with COVID-19 lately, it’s not just you. COVID-19 is on the upswing in many states.
As of September 5, the Centers for Disease Control and Prevention (CDC) estimated that infections were still growing or likely growing in 24 states*. Data also showed COVID-19 test positivity increased by 10.8%* over the previous week.
This uptick in infections is largely driven by a new COVID-19 variant called XFG, or “Stratus”.
Looking to find out more about XFG? Here are five things to know about this new variant.
1. XFG Has Spread Rapidly
According to a report in the scientific journal Lancet, XFG has spread rapidly across the globe after it was first detected. The United States is no exception to this trend.
In June, The World Health Organization (WHO) classified XFG as a “variant under monitoring.” Simply put, this means that XFG needed additional monitoring because it has mutations that could lead to improved growth or transmission.
As of the end of August, the CDC estimated that XFG was responsible for 78%* of COVID-19 illnesses in the United States. At the beginning of September, it was also the predominant COVID-19 variant* found in wastewater samples across the country.
2. XFG Doesn’t Cause New Symptoms or More Severe Illness
When it comes down to symptoms, there’s no evidence that XFG differs significantly from other recent COVID-19 variants. According to the CDC, general COVID-19 symptoms to look out for still include:
-
Fever
-
Chills
-
Fatigue
-
Cough
-
Shortness of breath
-
Sore throat
-
Headache
-
Body aches and pains
-
Runny or stuffy nose
-
Loss of taste or smell
-
Digestive symptoms like nausea, vomiting, or diarrhea
A WHO report noted that data on XFG doesn’t indicate that it leads to more serious illnesses or to more deaths compared to other circulating COVID-19 variants. This is supported by CDC data* that shows only slight increases in ER visits and hospitalizations over the past few weeks.
3. XFG Emerged Through A Process Called Recombination
Generally speaking, new variants of SARS-CoV-2, the virus that causes COVID-19, come about as the virus racks up mutations.
Viruses are obligate parasites, meaning that they require a living cell in order to reproduce. While replicating inside a host cell, changes in the genetic sequence of a virus, called mutations, can happen naturally.
Some mutations can be beneficial to the virus, such as by boosting its growth or helping it to better escape our immune system. When this happens, a new variant can have an advantage over other circulating variants and may eventually become the dominant variant.
XFG emerged using a slightly different path. When scientists analyzed XFG’s genetic sequence, they found that it was a recombinant of two prior COVID-19 variants.
In simple terms, this means that these two variants shared genetic material while present in the same host cell. The result was XFG, which has a genetic sequence that’s a mishmash of the two variants.
4. New Variants Spread Quickly Due to Advantages Over Current Variants
As mentioned earlier, new variants can have changes in their genetic sequence that give them an edge over current variants. This is what allows them to spread so quickly.
Indeed, an analysis of XFG found that it has a growth advantage when compared to other recent variants.
It also appears that XFG is better at escaping the immune system, meaning that antibodies from a prior infection or vaccination may not protect as well against it.
Despite its advantages in growth and immune escape, XFG actually binds less well to its receptor than other recent variants. That means that once inside the body, it may not be able to enter host cells as effectively.
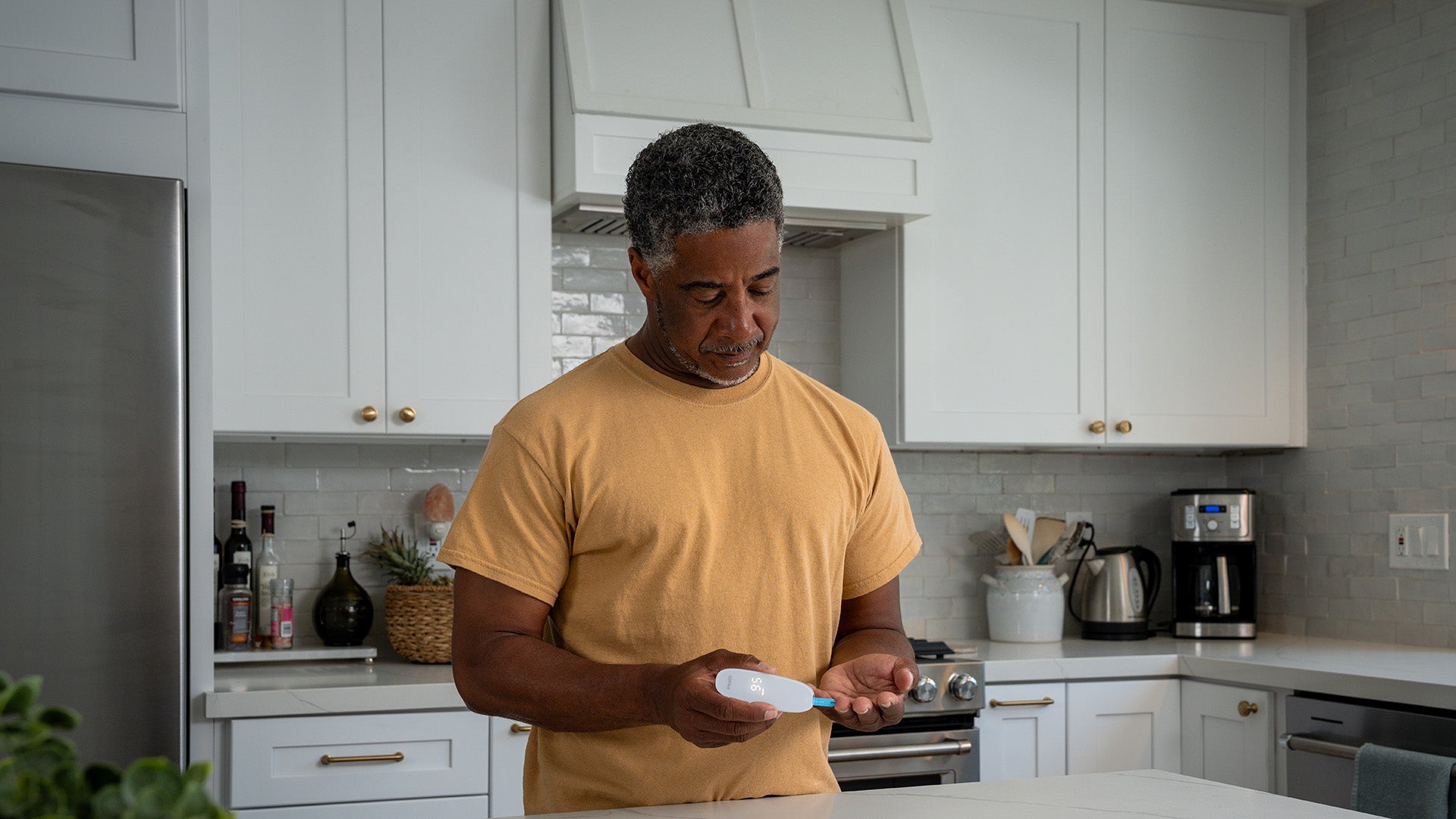
5. At-Home Tests Can Still Detect New Variants
With this bump in COVID-19 cases, you may be wondering if at-home tests can still detect XFG and other newer variants.
The good news is that studies conducted across the globe have found that rapid antigen tests are generally effective at detecting a variety of COVID-19 variants.
That means that if you’re concerned you may have COVID-19, taking an at-home test is a great first step!
The Food and Drug Administration (FDA) recommends testing immediately if you have COVID-19 symptoms. If you were around someone with COVID-19 but do not yet have symptoms, the FDA advises to wait at least 5 full days before testing.
When it comes to test results, the FDA notes that you can safely assume you have COVID-19 if you get a positive result on an at-home test. However, they recommend testing again after 48 hours if you get a negative result at first.
Positive Test? Here’s What To Do
If you do end up with a positive COVID test, the CDC recommends staying home until both are true for at least 24 hours:
-
Your symptoms are improving
-
You haven’t had a fever (and aren’t using a fever-reducing medication)
Also keep in mind that, in addition to at-home care like rest, hydration, and over-the-counter medications, antiviral treatments are available for people who are at risk of serious illness due to COVID-19.
Antiviral regimens generally work best when started 5 to 7 days after you get sick, so be sure to reach out to your doctor promptly after a positive test.
Additional References
-
ASM Journals: Comparison of the analytical and clinical sensitivities of 34 rapid antigen tests with prevalent SARS-CoV-2 variants
-
CDC: Current Epidemic Trends
-
CDC: Surveillance and Data Analytics
-
CDC: Variants and Genomic Surveillance
-
CDC: National Wastewater Surveillance System
-
CDC: Preventing Spread of Respiratory Viruses When You’re Sick
-
CDC: Symptoms of COVID-19
-
CDC: Covid Treatment Clinical Care for Outpatients
-
CDC: People with Certain Medical Conditions and COVID-19 Risk Factors
-
National Library of Medicine: Comparative evaluation of RT-PCR and antigen-based rapid diagnostic tests
-
FDA: At-Home COVID-19 Diagnostic Tests: Frequently Asked Questions
-
National Library of Medicine: Recombination in Viruses
-
National Library of Medicine: SARS-Co-V2 Variants
-
The Lancet: Infectious Diseases
-
WHO: Risk Evaluation for SARS-Co-V2 Variant Under Monitoring
-
WHO: Updated Working Definitions and Primary Actions for SARS-Co-V2 Variants
*The CDC updates states’ COVID-19 data weekly and other related data on a recurring basis. Any CDC data cited in published articles is the most current data as of the time of publishing.
Sign Up For More From iHealth
Receive the Latest News and Special Offers