Learn Your Way
to A Healthier Life

Are you getting too little sleep? Conversely, you might also be getting too much sleep.
Believe it or not, studies have shown that both of the above conditions could have an adverse effect on your blood pressure. High blood pressure (hypertension) affects almost 50% of adults in the US and is a major risk factor for cardiovascular disease.
Sleep is a critical physiological activity–the average person spends about one-third of their life sleeping–that’s 26 years for someone who has a lifespan of 80 years. It is so critical to health that the American Heart Association (AHA) added sleep health to its “Life’s Essential 8,” a checklist of key measures for improving and maintaining cardiovascular health.
The Sleep Sweet Spot
The amount of sleep that one needs varies significantly by age and even from individual to individual, but The National Sleep Foundation, American Heart Association, and CDC all recommend that for adults 18+ years old, 7-9 hours of sleep per night generally is the ideal for optimal health.
Sleep helps the body to regulate the hormones needed to control stress and metabolism. Over time, sleep deprivation can cause swings in these hormones–which can lead to high blood pressure and other risk factors for heart disease. Significantly, if a person already has high blood pressure, not getting enough sleep could make it even worse.
Research published in the AHA Journal Hypertension found the following:
-
Adults who got less than seven hours of sleep per night have a 36-66% higher risk of hypertension
-
Adults who got more than nine hours of sleep per night have a 11-30% higher risk of hypertension
Besides high blood pressure, consistently getting less than seven hours or more than nine hours of sleep a night is also associated with significant risks of other chronic health conditions including obesity, type 2 diabetes, and cardiovascular disease.
Also in the Blood Pressure Danger Zone: Erratic Sleep Schedules
In addition to the number of hours that one sleeps, the Hypertension study also found that irregular sleep schedules are linked to high blood pressure. People who varied the times they went to sleep and woke up throughout the week, even if they managed to get the recommended amount of hours each night, were still more likely to have a higher risk of hypertension than those with more consistent sleep routines:
-
Adults whose bedtimes varied by 90 minutes or more faced 92% increased odds for high blood pressure, compared to those who stuck to a regular bedtime
-
Adults whose bedtimes varied by only slightly more than 30 minutes from night to night were 32% more likely to have high blood pressure
-
Adults whose sleep duration varied by more than two hours or more from night to night had a 85% higher risk of hypertension than those who had less than an hour’s difference
Consistently going to sleep and waking up at the same time every day is just as crucial to blood pressure health as getting the recommended nightly 7-9 hours of sleep– and study data suggests that a consistent sleep schedule could even be more significant than number of hours slept.
Not only is it a good practice so that blood pressure is not adversely affected, a consistent sleep schedule also regulates one’s natural sleep-wake cycle, known as the circadian rhythm. This can lead to improved sleep quality, increased alertness, and overall well-being.
First Steps to a Sleep Schedule
There is a myriad of advice and tips out there on how to get the hours of sleep one needs as well as how to get on a consistent slumber schedule. The National Sleep Foundation recommends three basic, but crucial first steps that can help one set and stick to a sleep schedule:
-
Prioritize sleep. Of course “sticking to a regular sleep schedule” is easier said than done. Even with the best intentions of doing so, hectic work schedules and other commitments can cause anyone to stray off course. But when sleep is truly valued and the health benefits of getting enough sleep is understood as well, maintaining a consistent sleep schedule can come more easily.
-
Use bedtime reminders and wake-up alarms. As it gets closer to your normal bedtime, use a reminder that it is time to start getting ready for sleep. In the morning, don’t oversleep by using a wake-up alarm.
-
Stick to a nightly wind-down routine. This is a simple nightly routine to let your mind and body prepare for sleep about 20-30 minutes beforehand with a relaxing activity such as writing in a journal, listening to soothing music or meditating. A consistent wind-down routine every night can aid in a consistent sleep schedule.
Besides the basic tips for setting a sleep schedule, individuals should also talk to a healthcare professional for additional support and aids if they are not getting enough sleep, especially if they already have high blood pressure–as poor sleep will just exacerbate the already serious chronic condition.
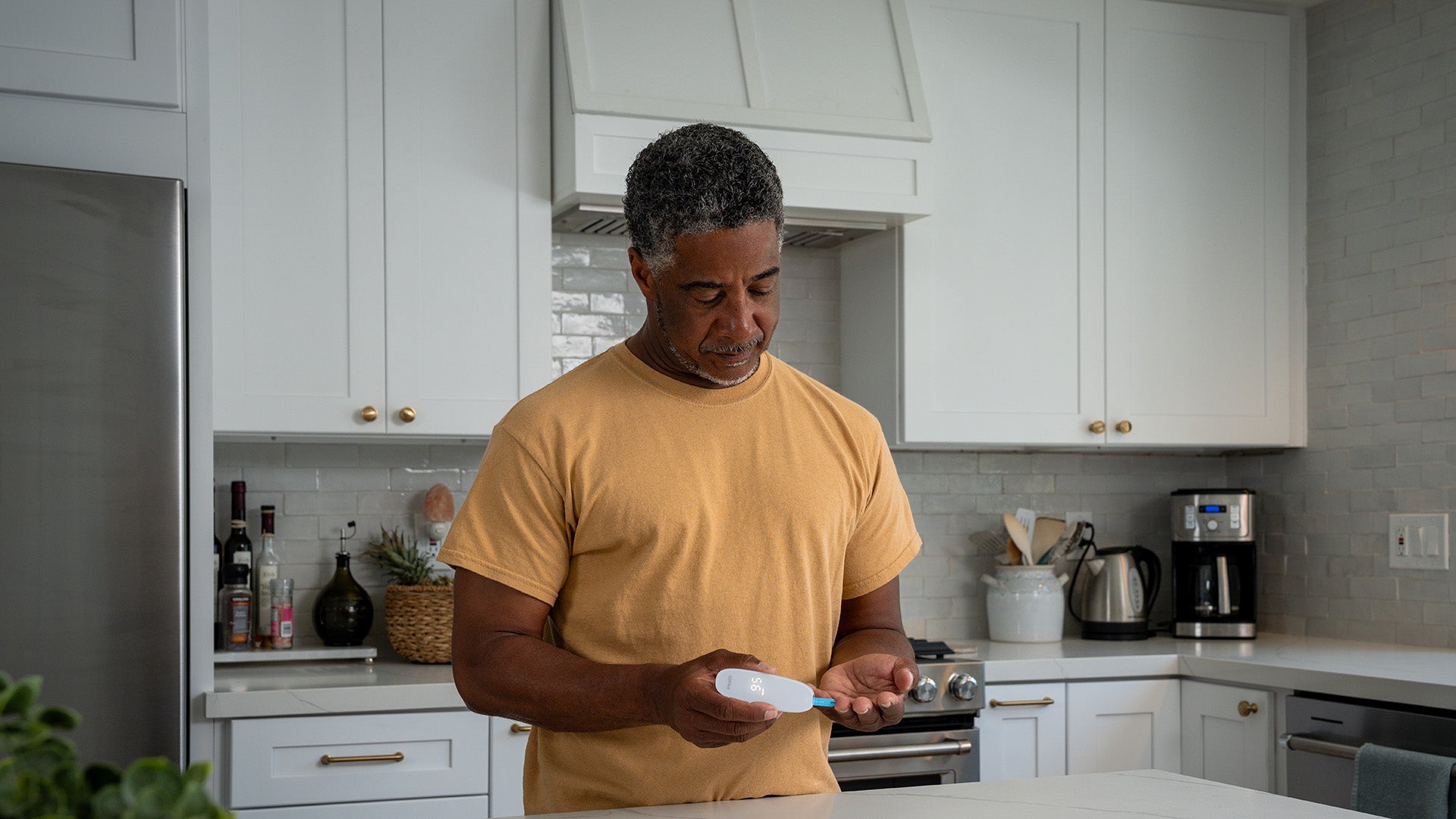
Blood Pressure Monitoring as Motivation? Yes
Studies suggest that at-home blood pressure monitoring, when combined with lifestyle adjustments, can lead to better blood pressure control.
At-home blood pressure monitoring can also be a useful tool in identifying and managing sleep-related issues that could affect blood pressure and overall health. By monitoring blood pressure, especially at night, individuals can get insights into potential sleep disorders such as sleep apnea and irregular sleep patterns, which can then be addressed through lifestyle changes or medical interventions.
Additionally, by monitoring regularly at home with the guidance of their doctor, individuals can get a comprehensive understanding of their blood pressure readings over time. This might be helpful for someone who has borderline blood pressure and can improve it gradually by adopting better sleeping habits, among other changes.
When people can see tangible results such as blood pressure improvements due to their efforts to make lifestyle changes, it can serve as motivation and encouragement to stick to those changes–such as that hard-to-come-by consistent sleep schedule.
-
American Heart Association: Irregular Sleep Schedule Linked to High Blood Pressure
-
Columbia University: How Sleep Deprivation Affects Mental Health
-
Mayo Clinic: Sleep Deprivation a Cause of High Blood Pressure?
Sign Up For More From iHealth
Receive the Latest News and Special Offers