Learn Your Way
to A Healthier Life

When we think of COVID-19, its physical symptoms typically come to mind. From coughing up a storm to not being able to taste or smell your dinner, dealing with COVID-19 can be pretty unpleasant.
One aspect of this infection that is not often discussed is how it may affect our mental health. Indeed, COVID-19 has been linked to a variety of mental health issues, particularly anxiety and depression.
With World Mental Health Day being observed today, let’s dive into five facts about COVID-19 and mental health to increase awareness of the connection between the two.
Fact #1: Rates of Depression and Anxiety Went Up During the Pandemic and Remain Above Pre-Pandemic Levels
Prior to the pandemic, a 2019 National Health Interview Survey (NHIS) report indicated that 10.8% of the U.S. population reported symptoms of anxiety or depression, two common mental health issues.
According to an 2024 analysis published in the International Journal of Environmental Research and Public Health, in the first year of the pandemic, the anxiety or depression rate shot up to 37.6%.
While this may not be a surprise in retrospect–it was an incredibly chaotic time after all–anxiety and depression rates in the recovery period post-pandemic still remain elevated and well above pre-pandemic levels, at 29.5%.
Fact #2: Having COVID-19 May Increase The Risk of Mental Health Issues
Early in the pandemic, researchers noticed an uptick in mental health issues in people recovering from COVID-19.
One 2022 review published in JAMA Psychiatry found that up to 90% of people who were hospitalized with COVID-19 and 25% of non-hospitalized individuals had at least one neuropsychiatric symptom, such as depression or a substance use disorder, in the six months after their illness.
A more recent study published in BMC Medicine supports this finding. It followed people who had recovered from COVID-19 for two years.
Compared to those who had not had COVID-19 during the same timeframe, these individuals had a higher risk of several mental health issues, including depression and anxiety, in the six months after they were ill.
Fact #3: It May Take Longer To Mentally Recover From COVID-19
If you’ve had COVID-19, it may take longer to recover mentally than physically. That’s the finding of a recent study from Open Forum Infectious Diseases that looked at physical and mental health after COVID-19.
This study found that physical health improved in most participants after three months. However, it took mental health nine months – three times longer – to bounce back.
Fact #4: People With Long COVID Have A Higher Risk of Mental Health Issues
Long COVID refers to a diverse collection of symptoms that last for three months or longer after you have COVID-19. People with long COVID also have a higher risk of mental health issues.
One recent study from Discover Mental Health found that individuals with long COVID were twice as likely to have depression or anxiety compared to those who experienced asymptomatic or mild COVID-19.
Long COVID can also affect the mental health of children. Another recent study published in Communications Medicine noted that pediatric long COVID significantly impacted quality of life and increased the risk of severe anxiety, depression, and sleep problems.
Fact #5: The Exact Reason Why COVID-19 Affects Mental Health Isn’t Clear
We don’t really know why people who’ve had COVID-19 are at a higher risk for mental health issues. It’s likely that multiple factors are at play.
For instance, the infection could impact the nervous system, leading to damage and boosting the risk of mental health issues down the road. Researchers have a few ideas about how this could happen:
-
Direct infection. The virus could be directly infecting and damaging parts of the nervous system.
-
Inflammation. The immune response to the infection could affect the nervous system. In fact, a small study published in JAMA Psychology linked markers of nervous system inflammation to depressive symptoms in people who had COVID-19.
-
Circulation issues. Circulation issues related to COVID-19 may reduce blood flow to the brain, increasing the risk of future mental health problems.
In addition to the infection itself, we can’t leave out other factors. For example, stress from being ill or hospitalized with COVID-19 or from coping with long COVID could absolutely play a role in developing conditions like depression or anxiety.
Many of the studies on COVID-19 and mental health include participants from early in the pandemic. As we can all remember, this was a time of social isolation, economic uncertainty, and fear of becoming ill. It’s certainly possible that all of these factors boosted the risk of mental health issues during that time.
Here’s How To Get Help
Mental health issues are very common. According to the National Institute of Mental Health (NIMH), more than one in five adults in the United States lives with a mental health condition.
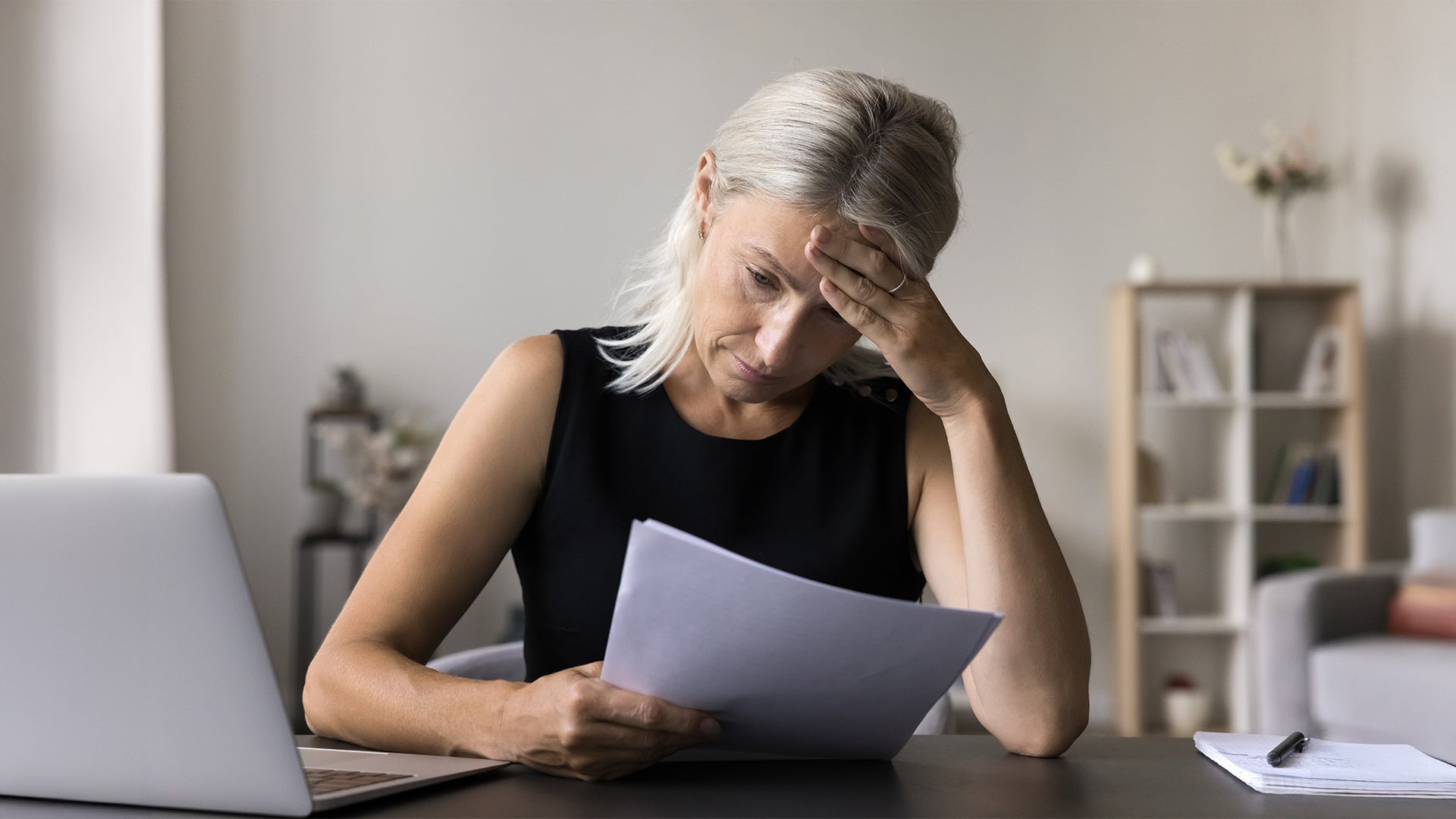
A few signs that could signal a mental health issue include:
-
Persistent feelings of sadness or anxiety that interfere with your life and daily activities
-
Decreased energy or loss of interest in activities
-
Trouble with concentrating or remembering things
-
Difficulty sleeping or oversleeping
-
Noticeable changes in appetite or weight
-
Physical symptoms like headaches or digestive issues that don’t have a clear cause
-
Recurring thoughts of death or suicide
Mental health issues shouldn’t be considered a stigma that you hide or just try to live with. If any of the above apply to you, reaching out to your primary care provider is a great first step. It’s pretty normal to feel nervous or self-conscious when discussing mental health concerns, but try to be as open and honest as you can.
An initial conversation with your PCP can pave the way for meeting with a mental health professional like a psychologist or psychiatrist. From medications to talk therapy, there are many effective treatment options for mental health issues.
In addition to contacting your PCP to chat about your concerns, the following resources may also be useful for getting help:
-
SAMHSA, the Substance Abuse and Mental Health Services Administration
-
The National Alliance on Mental Health (NAMI)
If you’re in crisis and need help immediately, don’t hesitate to contact the 988 Suicide & Crisis Lifeline by calling or texting 988 or by starting an online chat.
Additional References
BMC Medicine. Psychiatric and neuropsychiatric sequelae of COVID-19 within 2 years: A multinational cohort study
BMC Neurology: Long-term neurological and cognitive impact of COVID-19: A systematic review and meta-analysis in over 4 million patients
CDC: Long COVID basics
Communications Medicine: Quality of life and mental health in children with long COVID
Discover Mental Health: Assessing the effects of long-COVID on mental health in the United States: A population-based study
eNeurologicalSci: Neurological complications after COVID-19: A narrative review
International Journal of Environmental Research and Public Health: The COVID-19 pandemic and its effects on mental health—A before, during, and after comparison using the U.S. Census Bureau’s Household Pulse Survey
JAMA Psychiatry: Bridging knowledge gaps in the diagnosis and management of neuropsychiatric sequelae of COVID-19
JAMA Psychology: Neuroinflammation after COVID-19 with persistent depressive and cognitive symptoms
Journal of Cerebral Blood Flow & Metabolism: Cerebral blood flow alterations and host genetic association in individuals with long COVID: A transcriptomic-neuroimaging study
National Health Interview Survey: Estimates of Mental Health Symptomatology by Month of Interview: United States, 2019.
NIMH: Mental illness
NIMH: Tips for talking with a health care provider about your mental health
Open Forum Infectious Diseases: Association of SARS-CoV-2 with health-related quality of life 1 year after illness using latent transition analysis
Reviews in Medical Virology: Neuroinflammation in post COVID-19 sequelae: Neuroinvasion and neuroimmune crosstalk
WHO: COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide
Sign Up For More From iHealth
Receive the Latest News and Special Offers