Learn Your Way
to A Healthier Life

Why Summer Isn’t Free From COVID
Despite the sunshine and rising temperatures of the upcoming summer season, warmer weather alone does not guarantee safety from COVID-19. Unlike the flu, which typically peaks in winter, COVID-19 doesn’t follow a strict seasonal pattern. Now considered endemic, SARS-CoV-2 maintains a constant presence at baseline levels in the population, similar to other recurring viruses like the flu.
COVID-19 also tends to surge when social behaviors and environmental conditions favor transmission. A report from Johns Hopkins further explains that in addition to waning immunity and new variants, specific “summer” trends such as increased summer travel, large gatherings like weddings or festivals, and a general relaxation of precautions all contribute to the rise in COVID-19 cases during the summer.
During the summer months, people also often escape the heat by spending more time in enclosed, air-conditioned spaces like offices, travel hubs, restaurants and event venues. These settings can easily become “hot spots” where COVID case numbers can rise. A Multidisciplinary Digital Publishing Institute study from 2023 showed that airborne transmission indoors is 18.7 times higher than outdoor transmission.
The aforementioned behaviors, coupled with people moving between regions and congregating in high-traffic public places, create ideal conditions for viral transmission. That’s why public health experts from the California Department of Public Health continue to stress the importance of improving indoor air quality, encouraging the use of high-quality masks in close quarters and offering regular testing.
How Organizations Can Prevent COVID Outbreaks
Curbing COVID surges doesn’t require a return to lockdowns—a proactive and flexible approach can help keep workers safe without disrupting operations.
Fortunately, organizations of all types—from businesses and schools to summer camps and service programs—can access the tools and methods to protect their people while keeping operations running smoothly. By applying prevention strategies, they can significantly reduce the risk of transmission, promote well-being and continue serving their communities safely and effectively.
Here are some effective strategies organizations can implement this summer:
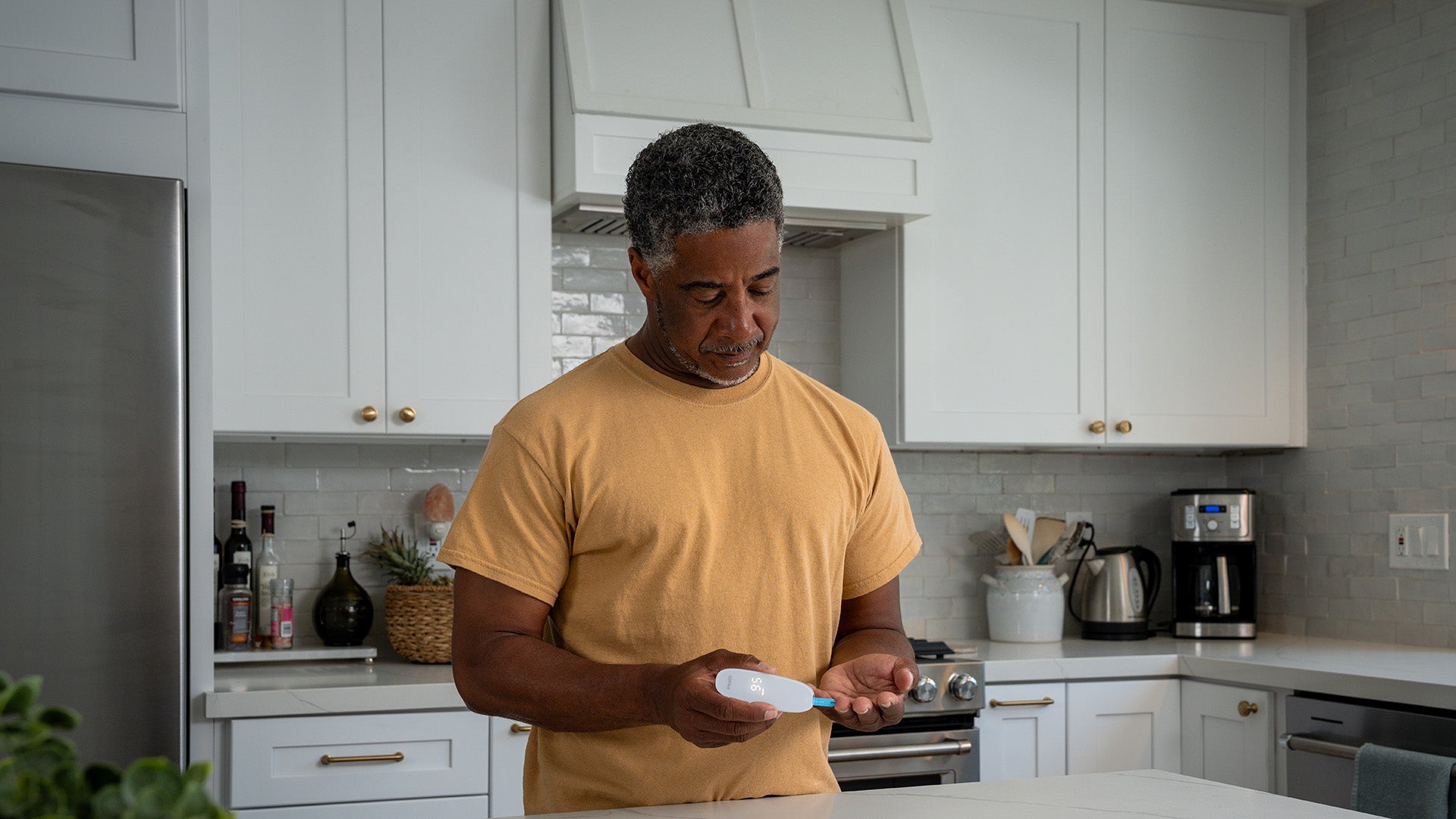
Use Rapid Testing Regularly
Modern rapid antigen tests help easily identify contagious individuals in just 15 minutes. The FDA now recommends people with noticeable symptoms (like fever or chills, cough, shortness of breath and sore throat) take at least two tests (one day apart). Even asymptomatic individuals with a known exposure should test multiple times. Organizations can offer voluntary testing for employees to monitor for symptoms—especially before and after large meetings or events or when staff return from travel.
For example, the Sierra Service Project, a Sacramento-based nonprofit known for its youth-led community service, is taking proactive steps for their summer 2025 program to prevent viral illness from disrupting their operations. Over the course of their nine‑week program, volunteers and staff live and work in close quarters while providing essential repairs for underserved residents—a setting that increases the risk of respiratory virus outbreaks.
iHealth recently supported Sierra Service Project's prevention efforts by donating flu and COVID-19 testing kits to the organization. With a twice-weekly testing schedule and additional screenings when symptoms arise, Sierra Service Project can quickly detect infections, distinguish between flu and COVID-19 and make timely decisions about isolating individuals or adjusting staff assignments. This approach helps protect their teams and their continued ability to serve vulnerable community members, including seniors and those with compromised immune systems, without introducing additional health risks.
Promote Vaccination and Boosters
Staying up to date on COVID-19 vaccinations remains the best way to prevent severe illness. The CDC currently recommends the updated 2024–2025 booster for everyone six months and older, with an updated version expected later this year. Organizations can support vaccination efforts by hosting on-site clinics, sharing reminders to get vaccinated or partnering with local health departments to provide access to vaccinations.
Improve Indoor Air Quality
The CDC also recommends upgrading HVAC (heating, ventilation and air conditioning) systems and installing HEPA (high efficiency particulate air) filters to help reduce airborne contaminants, including viruses, in a building or small space. Additionally, it is recommended to use portable air purifiers and increase outdoor air circulation with open windows to reduce the concentration of viruses in indoor spaces.
Encourage Using High-Quality Masks
UC San Francisco’s Peter Chin-Hong, MD, an infectious disease expert, recommends COVID- positive individuals use N95 or KN95 masks during the first 5-7 days after infection—when viral load transmission is at its highest—to prevent spreading the virus to others, especially in indoor environments. Dr. Chin-Hong also advises that when COVID-19 levels in state and regional wastewater rises, masks should be worn on public transport, in airports or any healthcare and eldercare settings.
Since COVID-19 can surge any time of the year, especially in high-contact indoor settings, summer is not a time to let protective measures lapse. Whether working in an office, out in the field or directly with community members—organizations can manage risk while remaining fully engaged in their missions. Prioritizing safer environments, monitoring team health and preventing the spread of infection can help them achieve their goals this season while safeguarding employee well-being.
References
- Harvard School of Public Health - Experts say COVID-19 is endemic. What does that mean?
- CDC - COVID-19 can surge throughout the year
- Multidisciplinary Digital Publishing Institute - Airborne Transmission of SARS-CoV-2: The Contrast between Indoors and Outdoors
- Johns Hopkins - Why COVID Surges in the Summer
- California Department of Public Health - Reduce Risk of Respiratory Infections by Improving Indoor Air Quality
- CDC - CDC Recommends Updated 2024-2025 COVID-19 and Flu Vaccines for Fall/Winter Virus Season
- CDC - Ventilation Can Reduce Exposure to Respiratory Viruses in Indoor Spaces
- UCSF - COVID-19 Masks: Expert Tips for What You Should (and Shouldn’t) Do
- FDA - Understanding At-Home OTC COVID-19 Antigen Diagnostic Test Results
-
CDC - Symptoms of COVID-19
Sign Up For More From iHealth
Receive the Latest News and Special Offers